A Patient-Centric Hemostatic Strategy
When planning surgery, patient factors including coagulation status and bleeding severity should be at the core of your hemostatic strategy.
Patient profiles are changing; increasing the risk of bleeding complications.1
15%
of US adults have chronic kidney disease.2
30%
of the US population use low-dose aspirin for cardiovascular disease prevention.3
~2/3
of surgical patients are treated with anticoagulants and/or antiplatelets.*4
*Based on Premier Database data
~1 in 50
adults have liver disease.5
~2 in 5
adults will be diagnosed with cancer in their lifetime.6

Patients at the core.
Each patient is unique, with their own set of factors that impact their risk of bleeding related complications.
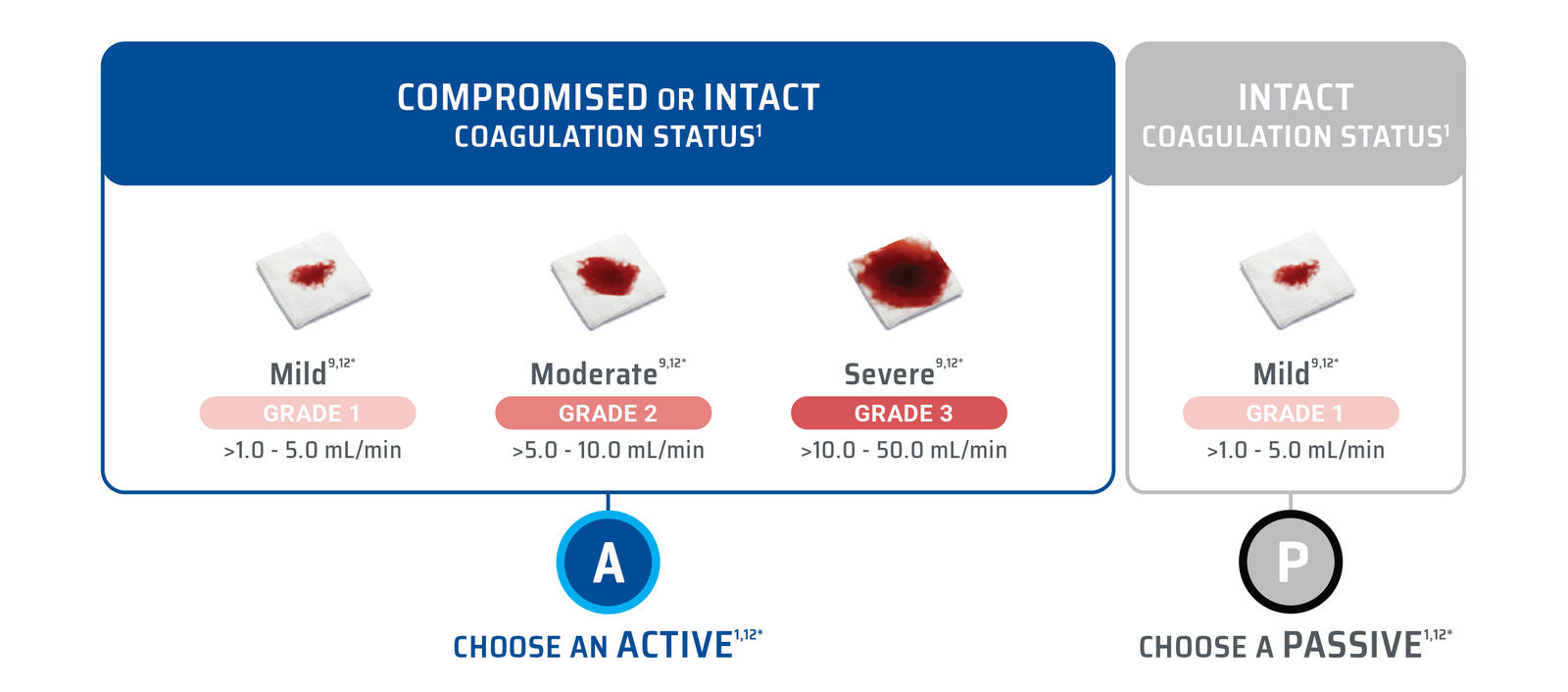
Some patients have an intact coagulation and relatively good health while others have compromised coagulation and existing comorbidities.
These factors can all influence the risk of bleeding7 and the performance of adjunctive hemostats agents and sealants.1
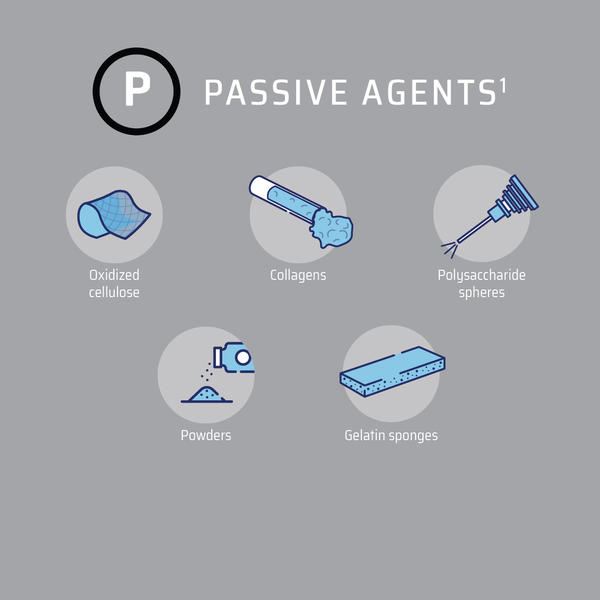
Passive hemostatic agents are effective in patients with intact coagulation.1
Active hemostatic agents are effective in patients with compromised and intact coagulation.1

The use of a validated bleeding scale could ultimately improve surgical efficiency by selecting the right adjunctive hemostatic agent for the right bleed. Choosing the appropriate adjunctive hemostatic agent may lead to:
Improved patient outcomes1,10
Fewer blood transfusions1,10
Reduced hospital costs1,10
Reduced length of hospital stay1,10,11
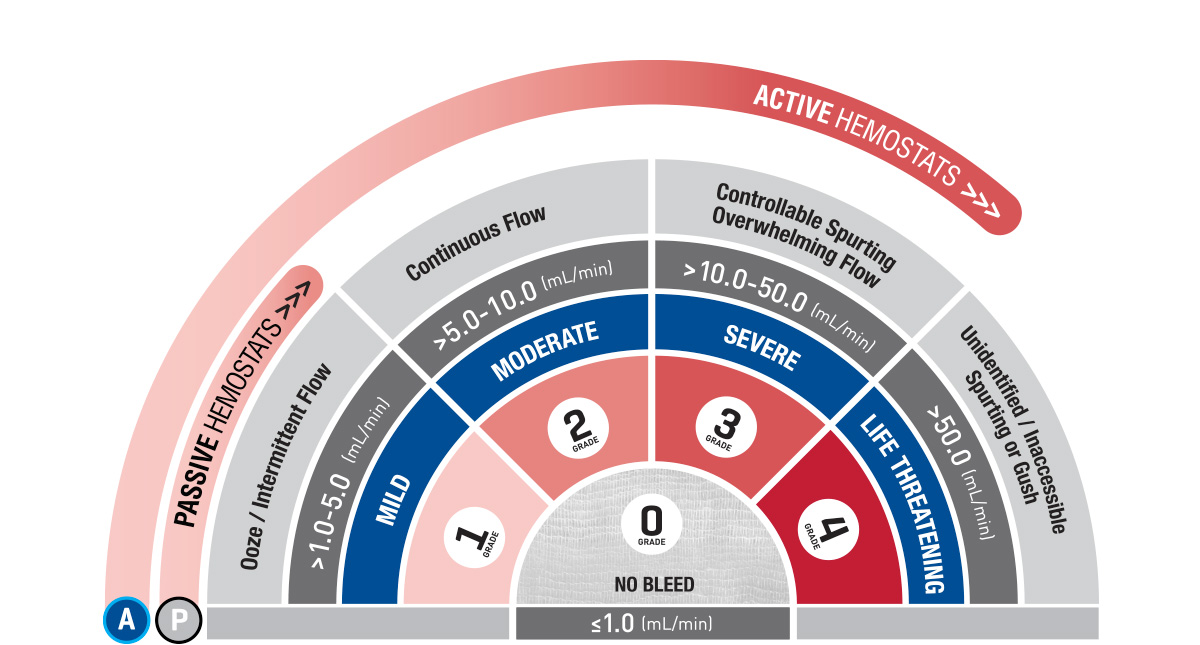
The VIBe SCALE tool is the first surgeon-validated FDA accepted scale designed for consistent and reliable assessment of intraoperative bleeding severity.9
Click the plus signs, below, to view videos of each grade of bleed.
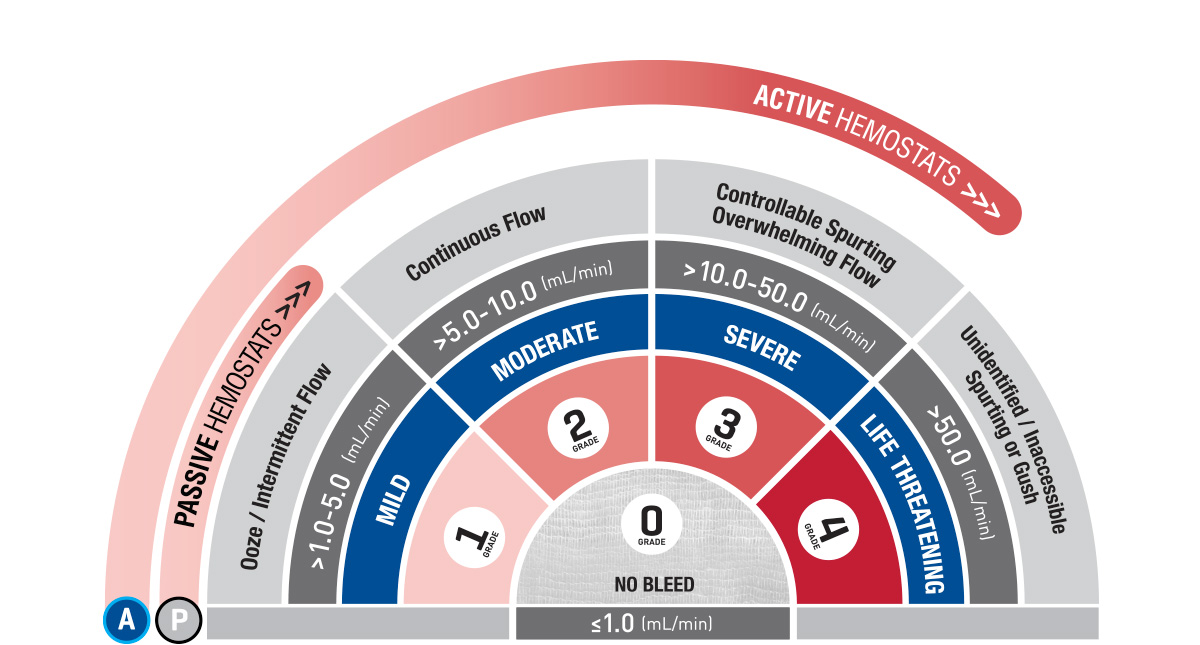
Grade 0: No Bleeding
- Superficial Nephric Abrasion
Grade 1: Mild
- Superficial Hepatic Abrasion
Grade 2: Moderate
- Superficial Cardiac Laceration
Grade 3: Severe
- Partial Hepatectomy
Grade 4: Life Threatening
- Supra-Renal Abdominal Aortotomy